Postpartum Depression Counseling Near Me: Expert Support for New Mothers

Understanding Postpartum Depression vs. Baby Blues in the Perinatal Period
The transition to parenthood brings profound changes that can challenge even the most prepared individuals. If you're searching for postpartum depression counseling near me, you're taking an important step toward prioritizing your mental health and well-being. While many new mothers experience some emotional adjustment during the postpartum period, understanding the difference between temporary baby blues and postpartum depression is crucial for recognizing when professional support becomes necessary.
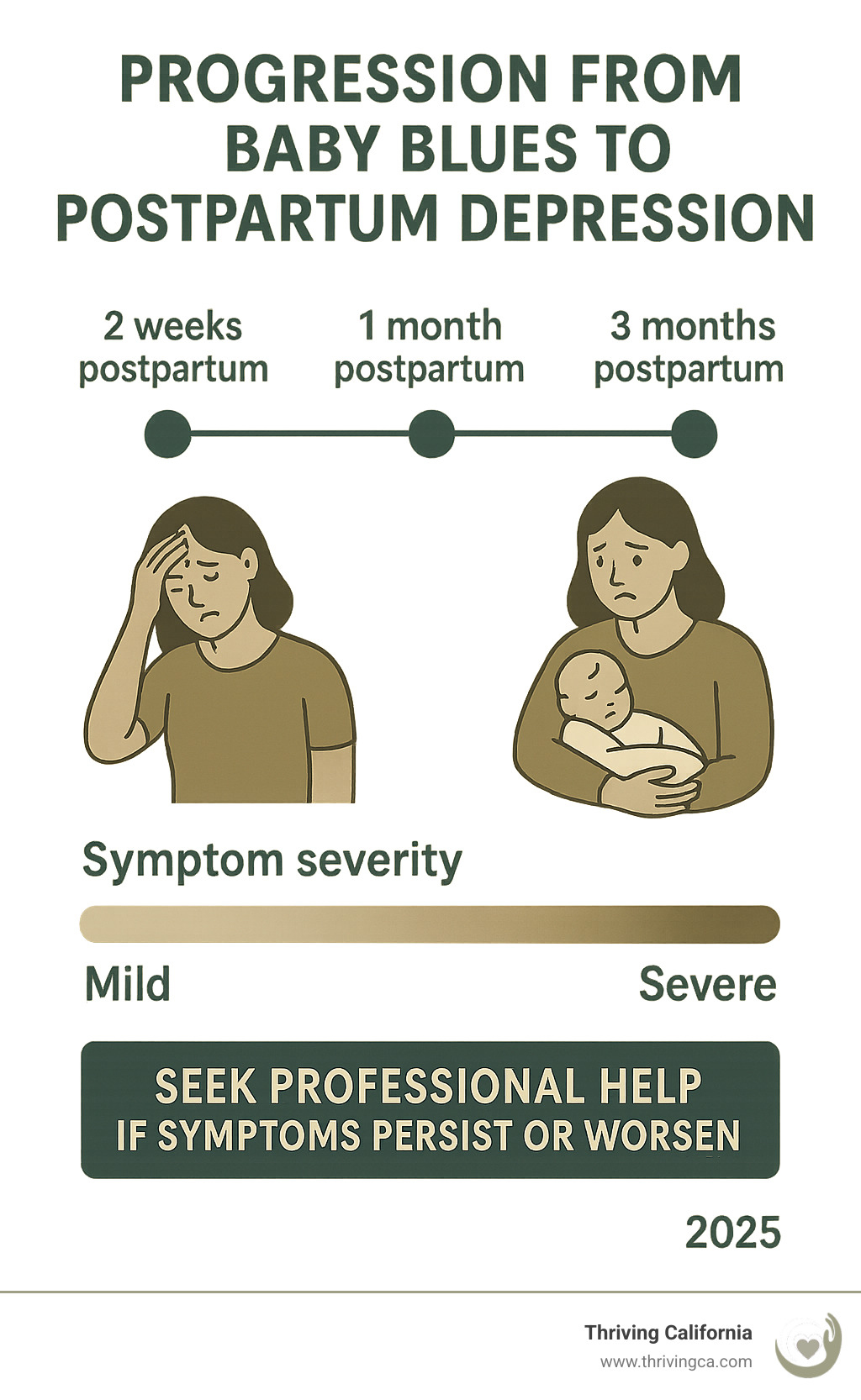
Baby blues typically begin within the first few days after giving birth and resolve within two weeks. These feelings are characterized by mood swings, crying spells, feeling overwhelmed, difficulty sleeping beyond normal newborn disruptions, and general irritability. These experiences affect approximately 80% of new mothers and are largely driven by dramatic hormonal changes, particularly the rapid drop in estrogen and progesterone after delivery.
Postpartum depression, however, represents a more serious and persistent mood disorder that can develop anytime within the first year after childbirth. This condition affects at least 1 in 7 mothers and requires professional intervention. Unlike baby blues, postpartum depression significantly impacts daily functioning and a mother's ability to care for herself and her baby. Many women also experience postpartum anxiety alongside depressive symptoms, creating complex perinatal mood and anxiety challenges that benefit from specialized care.
At Thriving California, our group practice of experienced therapists and doctoral-level clinicians specializes in perinatal mental health and maternal mental health support. Located near Napa, Lafayette, and Thousand Oaks, we also provide telehealth counseling sessions throughout California, offering personalized postpartum depression treatment that addresses the complex factors contributing to postpartum mental health challenges.
Recognizing Postpartum Depression Symptoms: When to Seek Professional Support
Understanding when normal postpartum adjustment crosses into clinical postpartum depression can help you seek timely treatment options. Key indicators include persistent ppd symptoms lasting more than two weeks that interfere with your daily functioning. Common symptoms of postpartum depression include both emotional and physical manifestations that many women experience during the postpartum period.
Emotional and psychological symptoms often include persistent sadness or depressed mood, severe postpartum anxiety or panic attacks, feelings of hopelessness or worthlessness, loss of interest in previously enjoyed activities, difficulty bonding with your baby, excessive worry about your baby's development, feeling like you've made a mistake becoming a parent, or intense feelings of guilt about your parenting abilities.
Physical symptoms may manifest as significant appetite changes, sleep deprivation beyond normal newborn-related disruptions, fatigue that doesn't improve with rest, unexplained physical aches and pains, headaches or stomach problems, or weight changes unrelated to normal postpartum recovery. These physical symptoms often accompany the emotional aspects of postpartum depression and require attention from mental health professionals.
Cognitive changes can include difficulty concentrating or making decisions, intrusive thoughts about harm, excessive worry about your ability to care for your baby, memory problems or feeling mentally "foggy," racing thoughts, or catastrophic thinking patterns. Some new mothers may also experience symptoms resembling postpartum OCD, with intrusive thoughts and compulsive behaviors that cause significant distress.
Behavioral changes might involve withdrawing from family members and friends, difficulty caring for yourself or your baby, increased irritability especially toward your partner, restlessness or feeling slowed down, avoiding previously enjoyed activities, or difficulty engaging with your baby. Feeling overwhelmed by simple daily tasks is another common indicator that postpartum depression treatment may be beneficial.
Trust your instincts about seeking support. If something feels different from your usual self or if these symptoms persist and interfere with your ability to function, postpartum depression counselors and other mental health professionals can make a significant difference in your recovery and overall well-being.
The Science Behind Perinatal Mental Health and Mood Disorders
Recent research reveals fascinating insights into what happens in the brain during pregnancy and the postpartum period. During pregnancy, your brain undergoes significant structural changes, particularly in areas responsible for empathy, anxiety, and social interaction. These neurological shifts are designed to help you bond with and protect your baby, but for some individuals, these changes combined with hormonal fluctuations can contribute to mood and anxiety disorders.
Postpartum depression involves disruptions in key neurotransmitters including serotonin (often called the "happiness chemical"), dopamine (important for motivation and pleasure), GABA (the brain's primary calming neurotransmitter), and oxytocin (the "bonding hormone"). Understanding these biological factors helps reduce self-blame and highlights why effective treatment from experienced therapists is both necessary and beneficial for maternal mental health.
It's important to distinguish postpartum depression from other perinatal mood conditions. While postpartum depression and postpartum anxiety often occur together, some women may experience postpartum psychosis, a rare but serious condition requiring immediate medical attention. Additionally, women with a family history of bipolar disorder may experience mood episodes during the postpartum period that require specialized care from healthcare providers familiar with these complex conditions.
The encouraging news is that these brain changes are treatable and often reversible with appropriate intervention. Therapeutic approaches that address both psychological and somatic aspects can help restore healthy brain function and neurotransmitter balance, supporting long-term mental health and well-being.
Risk Factors and Contributing Elements
Certain factors can increase the likelihood of developing postpartum depression or other perinatal mood disorders. Biological risk factors include previous history of depression, anxiety disorders, or other mental health conditions, family history of mood disorders including bipolar disorder, hormonal fluctuations and thyroid dysfunction, complications during pregnancy or delivery, premature birth or baby's health problems, breastfeeding challenges, or traumatic birth experience.
Psychological risk factors encompass unplanned pregnancy, strained relationships or lack of partner support, financial stress or major life changes, history of trauma or abuse, perfectionist tendencies or unrealistic expectations about motherhood, previous pregnancy loss or fertility struggles, concerns related to previous mental health challenges, or unresolved trauma that surfaces during the vulnerable postpartum period.
Social and environmental factors include lack of a strong support system or isolation, cultural or family pressure about parenting, work-related stress, housing instability or major life transitions, sleep deprivation that exceeds normal newborn care challenges, or caring for other children or family members while adjusting to new parenthood.
Having risk factors doesn't guarantee you'll develop postpartum depression, and many women without obvious risk factors still experience perinatal mood and anxiety challenges. Mental health conditions don't discriminate based on income, education, or how prepared you feel for parenthood.
Therapeutic Approaches for Postpartum Depression Treatment
Our group practice offers evidence-based treatment options specifically tailored to the unique needs of new mothers and pregnant women experiencing perinatal mental health challenges. Each approach is personalized to address your individual circumstances and therapeutic goals, helping women navigate this complex transition with professional support.
Psychodynamic Therapy focuses on developing a deeper understanding of how past experiences and unconscious patterns influence your current struggles with postpartum depression. This approach proves particularly helpful for exploring how your own upbringing affects your parenting, understanding relationship patterns that may contribute to depressive symptoms, and processing complex emotions about motherhood and identity changes.
Relational Therapy emphasizes the importance of relationships in healing and growth. For new mothers, this involves improving communication with your partner, addressing changes in family dynamics, building stronger support systems that sustain long-term mental health, and helping family members understand how to provide encouraging support during your recovery.
Internal Family Systems Therapy helps you understand different parts of yourself and how they interact during this significant life transition. This proves especially valuable for managing conflicting intense feelings about motherhood, addressing self-criticism and perfectionism, and integrating different aspects of your evolving identity as both an individual and a parent.
Birth Trauma Therapy utilizing somatic resourcing and bilateral stimulation specifically addresses traumatic birth experiences that can contribute to postpartum depression. This specialized approach, typically completed in 3-6 sessions for individuals and 6-12 sessions for couples, helps process traumatic birth experiences, reduce physical symptoms of trauma, and restore a sense of safety in your body. We work through your birth story starting from conception and pregnancy, moving through the birthing experience and into the postpartum period.
Our postpartum depression therapists are informed by Gottman principles for couples work, though we adapt these concepts to meet your specific relational needs rather than following rigid protocols. This flexibility allows us to provide effective treatment that honors your unique circumstances and relationship dynamics.

What to Expect: The Counseling Process
Understanding the treatment process can help reduce anxiety about beginning postpartum depression counseling. Our intake process typically begins with booking a consultation through our Calendly system. During this conversation, we learn about what you're looking for in postpartum depression treatment to determine if we're a good fit. If we're not the right match for your specific needs, we provide appropriate referrals to other mental health professionals. If we are a good fit, we discuss logistics including scheduling your counseling sessions and fees, leaving ample time for your questions.
For those ready to begin without a consultation, we can use the first session to assess fit and begin the therapeutic work. You'll register in our Simple Practice system where you'll complete our brief intake form. Telehealth clients receive secure session links through this platform, making it convenient to access postpartum depression counseling from the comfort of your home.
Your first session involves gathering information about your pregnancy, birth experience, and current postpartum depression symptoms. Together, we identify treatment goals and discuss how our therapeutic approach addresses your specific mental health needs. You'll have ample opportunity to ask questions about the process and what to expect as we work together on your recovery.
For ongoing psychodynamic and relational work, we typically meet weekly in 50-minute sessions, though frequency can be adjusted based on your needs and circumstances. In initial sessions, we're gathering information and building our therapeutic relationship. Once established, you can expect to explore the aspects of your life that feel most important and relevant to your treatment goals. Sometimes this means examining childhood experiences or past relationships; other times it focuses on current relationships and stressors. We follow your lead regarding what feels most relevant while providing guidance and insights to support your growth and well-being.
For birth trauma work, we start with your birth story from conception and pregnancy, moving chronologically through your experience. As we work through your story using specialized coping strategies, you'll likely experience a reduction in trauma symptoms and associated postpartum depression. By the end of our work together, the birth story typically becomes much less triggering, often measuring 1-2 on a 10-point distress scale compared to the higher levels experienced initially.
Progress markers include improved sleep quality beyond normal newborn disruptions, increased energy and motivation, better appetite regulation, improved bonding with your baby, enhanced communication with your partner, reduced anxiety about parenting decisions, decreased feeling overwhelmed by daily tasks, and greater self-compassion and acceptance of yourself as a developing parent.
Building Support Beyond Individual Sessions
While postpartum depression counseling provides crucial support, healing happens between sessions too. Building a comprehensive support system enhances your recovery and long-term mental health resilience for both new mothers and their families.
Partner and family involvement can include sharing insights from therapy using specific, actionable language, helping your partner understand concrete ways they can support your mental health, communicating your needs clearly regarding visitors and household responsibilities, and considering couples sessions to address relationship dynamics and improve mutual understanding. Many family members benefit from education about postpartum depression to provide more effective and encouraging support.
Daily coping strategies and self care might involve parent-baby bonding exercises like skin-to-skin contact during feeding times, mindful observation of your baby's cues without judgment, gentle touch and massage to promote connection, talking and singing to your baby even if it feels awkward initially, reading together to create positive interactions, and incorporating the baby into gentle movement activities that support your mental health.
Practical support for daily challenges includes sleep hygiene strategies that work with newborn schedules while addressing sleep deprivation, nutrition planning for busy new mothers focusing on easy, nutrient-dense options, gentle movement appropriate for postpartum recovery, mindfulness practices you can do while caring for your baby, time management techniques that account for unpredictable newborn care, and energy conservation strategies to help prioritize essential tasks when feeling overwhelmed.
Mental health maintenance involves mood tracking to monitor your progress with postpartum depression symptoms, gratitude practices adapted for the challenges of new parenthood, breathing exercises that can be done anywhere to manage postpartum anxiety, progressive muscle relaxation for physical symptoms of tension and anxiety, cognitive restructuring techniques to challenge negative thought patterns, and grounding exercises for moments of intense feelings or panic.
Professional Resources and Community Support
Community resources can complement your postpartum depression treatment and provide additional layers of support. Consider connecting with new parent groups that provide peer connection and practical advice for postpartum women, working with postpartum doulas for additional practical and emotional support, consulting with lactation specialists for breastfeeding challenges that may contribute to stress, exploring parent-child classes that promote bonding and reduce isolation, and connecting with religious or spiritual communities that offer support and understanding.
Digital support options include Postpartum Support International online resources for perinatal mental health, apps designed for new mothers that provide community and symptom tracking capabilities, and telehealth opportunities that allow you to connect with specialized postpartum depression counselors regardless of geographic location.
Professional team expansion might include your primary care physician for overall health monitoring, your OB/GYN for postpartum physical recovery and hormonal considerations related to women's health, your pediatrician who understands family mental health dynamics, and potentially a psychiatrist if medication consultation becomes necessary to support your postpartum depression treatment.
It's important to have a healthcare provider who understands the complexity of perinatal mood disorders and can coordinate your care effectively. This integrated approach ensures that all aspects of your physical and mental health are addressed during your recovery.

Specialized Training and Credentials
When seeking postpartum depression counseling near me, it's important to work with mental health professionals who have specialized training in perinatal mental health and maternal mental health. Our team of experienced therapists holds doctoral-level degrees and has extensive experience helping women navigate the challenges of postpartum depression and related mood and anxiety disorders.
Look for postpartum depression counselors who understand the unique aspects of perinatal mood conditions, including how postpartum depression differs from general depression, the impact of hormonal changes on mental health, the importance of the mother-baby relationship in recovery, and how to address trauma related to pregnancy, giving birth, or early parenting experiences.
Our specialized training allows us to provide effective treatment that addresses not only the symptoms of postpartum depression but also the underlying factors that contribute to perinatal mental health challenges. This comprehensive approach supports lasting recovery and improved well-being for both mother and baby.
Insurance and Practical Considerations
At Thriving California, we work with out-of-network benefits, which often provide more flexibility in choosing your postpartum depression therapist and treatment approach. We encourage you to contact us for specific information about fees and how to maximize your out-of-network benefits for postpartum depression counseling.
Our 50-minute counseling sessions provide adequate time to address complex issues while maintaining clear boundaries that support the therapeutic process. We use Simple Practice's secure platform for both scheduling and telehealth sessions, ensuring your privacy and confidentiality are protected throughout your postpartum depression treatment.
Crisis Resources and When to Seek Immediate Help
While postpartum depression is very treatable with appropriate care, it's important to recognize when immediate medical attention may be necessary. Postpartum psychosis is a rare but serious condition that can involve hallucinations, delusions, or paranoia after childbirth and requires immediate medical attention. If you experience thoughts of harming yourself or your baby, call 911 or seek emergency help right away.
Crisis resources include the 988 Suicide & Crisis Lifeline for 24/7 support, Postpartum Support International Helpline at 1-944-443-5754 for specialized perinatal mental health support, and your local emergency services if you're in immediate danger.
Having a safety plan developed with your postpartum depression counselor can help you recognize warning signs and know exactly what steps to take if you experience a mental health crisis. This planning is a standard part of responsible postpartum depression treatment.
Taking the First Step Toward Recovery
Searching for postpartum depression counseling near me represents a courageous step toward reclaiming your mental health and strengthening your connection with your baby. Postpartum depression is not a reflection of your worth as a parent—it's a treatable mood disorder that affects millions of individuals during this vulnerable time.
Our group practice of doctoral-level clinicians at Thriving California understands the unique challenges facing new mothers and pregnant women experiencing perinatal mood and anxiety disorders. We offer both in-person sessions near Napa, Lafayette, and Thousand Oaks, as well as telehealth counseling sessions throughout California, ensuring you can access specialized postpartum depression treatment regardless of your location or circumstances.
What sets our approach apart includes experienced therapists with specialized training in perinatal mental health, comprehensive treatment options addressing both individual and relational factors, flexible scheduling with both in-person and telehealth counseling sessions, personalized treatment approaches that evolve with your needs, and focus on breaking intergenerational patterns while building resilience for long-term well-being.
Ready to take the next step in seeking support? We encourage you to book a consultation through our Calendly system. During this conversation, we'll learn about your specific mental health needs, answer your questions about postpartum depression treatment, and determine if our approach aligns with your goals. If we're not the right fit, we'll provide appropriate referrals to ensure you receive the specialized care you deserve.
Seeking help isn't just about you—it's about your baby, your partner, and your entire family. When you prioritize your mental health during the postpartum period, you're modeling self care and resilience for your child while strengthening your family's foundation for lasting well-being.
Professional postpartum depression counseling, combined with your own strength and determination, can help you move through this challenging time toward a more connected, confident, and joyful experience of parenthood. Many women find that effective treatment not only addresses their immediate postpartum depression symptoms but also provides valuable coping strategies and insights that serve them throughout their parenting journey.
For more information about our specialized therapy services for perinatal mental health and maternal mental health support, visit our website or reach out directly. Postpartum depression is temporary, but the skills and insights you gain through treatment will serve you throughout your parenting journey and beyond, contributing to your overall well-being and that of your growing family.
